Abstract
Enabling universal access to high quality health information is challenging in multicultural Australia, where low proficiency in English can hinder access to information services. eHealth initiatives may potentially facilitate better access to health information for minority cultural groups. However, the extent to which ehealth initiatives are inclusive for culturally and linguistically diverse groups remains under-explored. A community survey was conducted to explore the extent to which members of a culturally and linguistically diverse community living on a public housing estate in Melbourne?s North, and the health professionals providing local community health services, currently used telecommunications in relation to health information. The community survey findings indicated relatively low levels of access to telecommunications in homes on the housing estate and infrequent use of the Internet to access health information. Health professionals used telecommunications for some forms of communication with patients but not others. The findings of this study have implications for the accessibility of electronic health information for culturally and linguistically diverse groups.
Introduction
eHealth in multicultural Australia
According to data from the 2011 Census, as at June 2010, 27% of Australia?s population were born overseas. A substantial proportion of the population was born in countries in which English is not the primary language. In the last ten years there have been considerable increases in the number of Australian residents who were born in Nepal, Sudan, Bangladesh, Zimbabwe and Pakistan (ABS 2011). Recent census data indicates that, as of 2006, 30.4% of 5.13 million recorded residents in the state of Victoria were born overseas (ABS 2006). This increasing cultural diversity, as well as the rapid population growth, the ageing population and rise in chronic disease, together with inequalities in health literacy make the provision of accessible health information and health services in Australia challenging. The demand for health services is increasing in growth areas and under-serviced locations. These locations are often highly populated with older residents likely to require aged care services and by migrant communities with diverse cultural and linguistic backgrounds (McGuirk and Argent 2011).
In Australia there is currently a move towards a health policy focusing on equipping health consumers with more information and power (Sillence et al. 2007). The National Health and Hospital Reform Commission report (NHHRC 2009) promotes a preventative self-management agenda. The Victorian state-based Department of Health presented a vision of community-led prevention to be realised through strong partnerships between primary health care and community health, aged care and other services. One example of such partnerships is the community health centres (CHCs). CHCs are based on the body of evidence that a strong community based primary health care system directly contributes to improved health status, reduced health inequalities and lower health system costs (Starfield 1994). The community health services model uses strong community connections and focuses on the underlying theory of the social determinants of health (Marmot 2005). Community health services where they exist, are often the first source of information about health services for many culturally and linguistically diverse (CALD) communities (Renzaho 2008) and are seen as an integral part of best practice for providing services for migrant communities (Woodland et al. 2010). In particular, screening and referral services are ideally provided in the community and services are designed to be culturally and linguistically appropriate, accessible and affordable (Woodland et al. 2010).
CALD migrant and ethnic communities in Western societies have traditionally had poorer health outcomes and access to healthcare than local communities due to barriers such as English language ability and cultural factors including health beliefs (Henderson et al 2011). Existing research on the potential and role of the Internet to address the disparity in health outcomes and access to healthcare and health information for CALD communities is limited. To navigate online health information, users require a combination of a high degree of English language competence including reading and numeracy skills as well as critical literacy to identify reliable health information. Conversely, when information is tailored to the user, online health information can assist users to formulate questions to ask their health professionals (Katz et al 2007). Therefore, the Internet has potential to assist CALD communities to overcome some of the barriers associated with accessing healthcare and improving health literacy (Rudd & Keller 2009).
Innovations in health services and the provision of health information
The demands for health care have been growing and changing and the explosion in digital developments worldwide has become an important part of the health agenda. Electronic and digital technology has been linked to coordination, integration and improving quality of health care (Victorian Department of Health 2009). This technology is also an essential carrier for information relating to health and health care, demanding intensive infrastructure development. In Australia, the National Broadband Network (NBN) will deliver infrastructure expected to provide significant support for the role of new technologies in health, resting upon the transferral of health information. For these developments to be inclusive for culturally and linguistically diverse communities, not only do considerations of Internet accessibility, literacy and eHealth literacy need to be taken into account, but also consumers? preferences and information-seeking behaviours for accessing health information have to be understood.
This study sought to contribute to the body of evidence on the use of telecommunications by CALD communities to access health information and to contribute to understandings of the role of telecommunications as an enabler of access to health information in different community contexts. The study?s main aim was to examine the access to, and use of, telecommunications by people of CALD backgrounds in relation to seeking health information. This exploratory study was a necessary starting point for considering the appropriateness of eHealth information strategies for improving health outcomes for under-represented communities.
Research design and methods
Design
A guiding principle of this study was to engage with the CALD community without becoming a burden or intruding in private environments, while also acknowledging the documented challenges of sampling migrant groups (Sulaiman-Hill and Thompson 2011). A community survey design involving the community identified was deemed the most respectful approach to engage and increase likelihood of participation. Community surveys are increasingly being utilised as an effective method for community-based research (Skinner et al. 1997). A community survey was selected over a case study because there were no suitable cases available for replication (Zainal 2007). The premise of a community survey approach is that engaging with a community is an effective and appropriate way to explore an aspect of community life. Unlike the case study method of gathering a range of artefacts to form a holistic interpretation of a phenomenon, a community survey makes use of a simple questionnaire survey tool and was seen to be appropriate for exploring a specific aspect of life for this community, in this case, access to telecommunications in the home in relation to health-information seeking behaviours (Colorado State University 2013). An exploratory community survey design was intended to act as a form of pilot study during investigation of what appeared to be the research problem and to support the identification of research questions for further study.
The community survey approach made use of existing relationships with organisations providing services to members of CALD communities within the North West Metropolitan region of Melbourne. This approach allowed researchers to build trust and familiarity with the research population by maintaining a presence at the CHC for four months. Relationships with key service providers working around and within the CHC were developed. This approach has been advocated for use where there might be ethical or political sensitivities in conducting the research (Skinner et al. 1997).
This paper relates the findings of the questionnaire component of the community survey.
Ethics
The research was given full ethical approval by the Human Research Ethics Committee at the University of Melbourne Participants were informed of their ethical rights in non-technical language and were given full information about the project before being asked to provide informed consent to take part. Participants were de-identified in the reporting of the research and only aggregate results were used.
Sampling and participants
As advised by local service providers, all research documents which were to be made available to participants were translated into the following languages, cross-referenced with demographic data about the Local Government Area (PHIDU 2011) to gain an insight into the demographic makeup of the area according to data stored locally:
- Traditional Chinese
- Vietnamese
- Sudanese Arabic
Towards the end of the project some documents were also translated into Hakka due to the prevalence of native Hakka speakers completing the surveys in English.
Participants were recruited from two population groups identified in the sampling criteria below.
Sampling criteria
|
Population Group 1 (n=59) |
Individuals who were present at the North Richmond Community Health Centre Individuals who self-select as having a first language other than English Individuals who are over the age of 18 |
|
Population Group 2 (n=64) |
Health professionals who currently work, or have previously worked with people from culturally and linguistically diverse backgrounds (eg. those with proficiency in a language other than English) Health professionals who currently work in a primary health care or community health setting |
Group 1
Advertisements for the study were translated into the languages listed above and were positioned in view of service-users visiting the Community Health Centre (CHC) site. The researchers visited the site in pairs twice a week for a four-month period and established a survey station positioning a desk in the foyer to the CHC and placing chairs on both sides of the desk. Surveys, advertisements and plain language statements were placed on the desks in piles according to translation.
Group 2
All staff in the CHC staff database were sent information and a plain language statement about the survey via the Centre Manager who had access to their email addresses. Health professionals were encouraged to forward the invitation to other health professionals in the region Health professionals were invited to consider completing the survey and were signposted to where the survey was available.
|
|
Surveys completed |
Surveys included* |
|
Group 1 participants (CALD) |
64 |
59 |
|
Group 2 participants (health professionals) |
64 |
64 |
Table 1 ? Number of valid surveys completed and returned.
*Group 1 surveys were excluded if the participants reported having no acquired languages other than English.
Study setting:
The CHC is situated at the bottom of the public housing estate which includes approximately 6,000 residents; approximately 70% are born in a non-English speaking country and a significant number arrived in Australia as refugees. In response to the linguistic diversity of the client group interpreters in Vietnamese and Chinese are employed, in addition all reception staff were bi-lingual and represented the ethnic communities that live on the estate.
Research instruments
The survey instruments were piloted with a small sample (n=7 in total). The survey instruments were then refined and the final two survey instruments were used in the main study (Appendix 1 & 2).
Procedure
Researchers were present while potential participants became familiar with the purpose of the research and began to feel comfortable in approaching the survey station and completing a survey. This meant that data collection required a patient and flexible approach. Findings are not generalisable and are not representative of other CALD communities.
Surveys
Survey questions were a combination of Yes or No responses, multiple choice, and Likert scale responses asking participants about the following topics:
- Access to telecommunications (landline, mobile phone, internet) in the home
- Frequency of use of telecommunications
- Competency and range of use of telecommunications
- Purpose of use of telecommunications: finding health information, contacting health services
On a number of occasions interpreters were present at the CHC. One of the interpreters was employed by the CHC and supported participants completing the surveys in Traditional Chinese. On one occasion during the data collection, the research team arranged for Hakka, Traditional Chinese, and Vietnamese interpreters to be available at the research site and to support the completion of surveys where needed.
Sample demographics
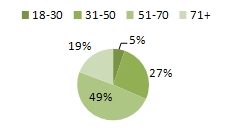
The majority of the 59 CALD survey respondents were aged 51 years or over (68%) and the mean age was 59 years. The relative older age of respondents may have been due to the times at which the researchers were available at the CHC to distribute and collect surveys. Researchers were present on week days only, between 09:30 and 16:00. The sample appeared representative of the community but in-depth community demographic data would be needed to substantiate this.
Figure 1 ? Age range of participants
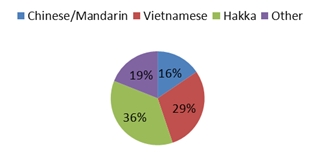
Figure 2 ? Participants? first language
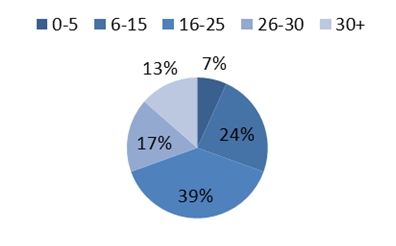
Figure 3 ? Length of time in Australia
Analysis of survey data
A descriptive, quantitative analysis was conducted of the survey data. The survey data was treated as two separate datasets: survey responses from people from CALD backgrounds (n=59) and survey responses from health professionals (n=64). The data sets were stored on an MS Excel spreadsheet and frequencies, averages and percentages were calculated using simple formulae. Each survey question was interrogated and key findings are presented in the Findings section.
Key Findings
People from culturally and linguistically diverse backgrounds
The demographic data indicated that the study sample was largely constituted by participants who had lived in Australia for two decades or more. A high proportion of these participants opted for surveys in their first language. There was a fairly even spread of languages spoken with Hakka being the most common first language reported (36%).
Access to telecommunications
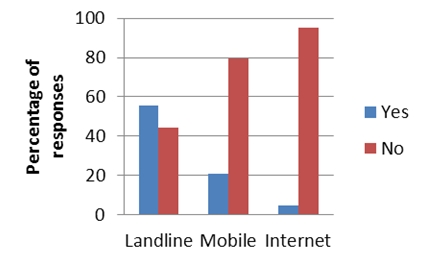
Most survey respondents reported having access to landlines (n=46 / 78%) and mobile phones (n=33 / 56%). Just over one quarter had access to the Internet (n=16 / 27%) and/or email (n=14 / 24%) in their homes. A total of 22 participants (37%) reported having home access to a landline telephone only. One participant reported having access to none of the four telecommunications categories. Only nine participants reported having access to all four (15%).
Figure 4 ? Access to telecommunications in the home
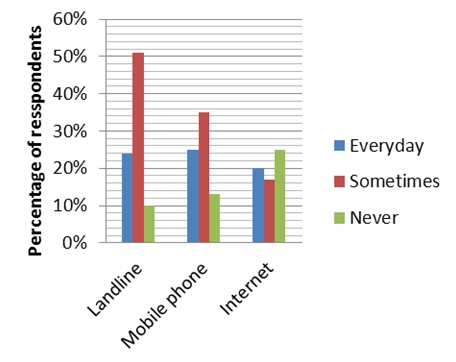
Figure 5 ? Frequency of use of telecommunications
Fifty one per cent of respondents reported using landlines some of the time (and 24 per cent did not use them every day. Mobile phone usage every day was slightly higher than every day use of landlines but overall access to mobile phones was lower. A quarter of the participants reported never using the Internet.
Use of telecommunications to access health information
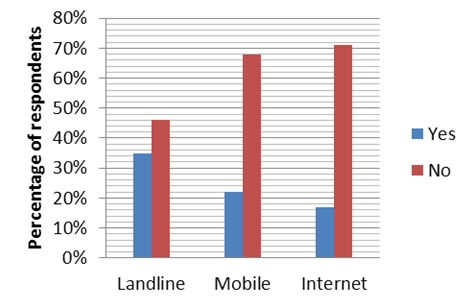
Approximately on third of the participants reported using landlines to find health information. Around 22% reported using mobile phones to find health information and only 16% (n=10) reported using the Internet to find health information. Most of the participants (n=42 / 71%) reported that they do not use the Internet to find health information.
Figure 6 ? Use of telecommunications to find health information
The survey data demonstrates that access to landlines and mobile telephones and the Internet is relatively low for this sample. It also demonstrates that use of telecommunications to access health information is not common practice but does exist among those who have access.
Health professionals working with CALD communities
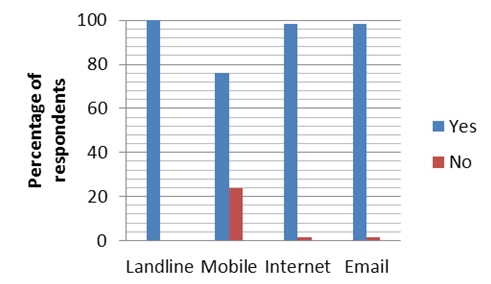
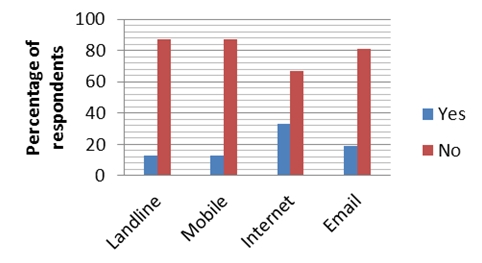
Approximately 63 per cent of the health professional participants were born in Australia. Seventy six percent had access to all four types of telecommunication mentioned in the survey: landline, mobile phones, Internet and email.
Figure 7 ? Access to telecoms in the workplace
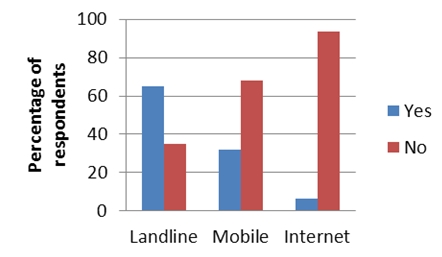
Health professionals were asked what they used telecommunications for in relation to communicating with, and providing information for patients and the community. As indicated in Figure 8, sixty five per cent reported using landlines to ask patients questions One third used a mobile phone for the same purpose and only 6% had used the Internet.
Figure 8 ? Use of telecommunications to ask patients questions
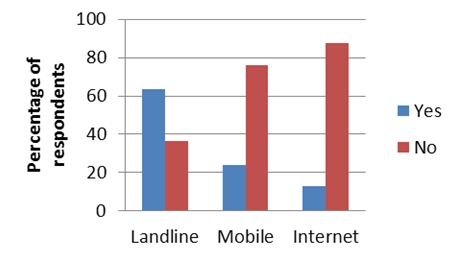
Figure 9 ? Use of telecommunications to arrange appointments with patients
As shown in Figure 9, similar proportion of health professionals reported using landlines to arrange appointments with patients (63%). Twenty three per cent had used mobiles for this purpose and 12% had used the Internet.
Figure 10 demonstrates that just over half the participants (55%) had used landlines to conduct consultations with patients. 20% reported using mobile phones for this purpose and 5% reported using the Internet.
Figure 10 ? Use of telecommunications to conduct consultations with patients
Figure 11 ? Health professionals? feelings about helpfulness of telecommunications when working with CALD patients
Discussion
The community surveyed appeared to have low access to the Internet in the home, when compared with the Local Government Area (27% Vs 84%) (Community Indicators Victoria 2011). There is very little literature on the access to and the use of the Internet and/or mobile phones by CALD users of community health services. A United States (US) study with a similar sample suggested that the use of Internet and/or mobile phones among this population group had been over-estimated (Denizard-Thompson et al. 2011). This may be due in part to the fact that ?ethnic minorities are under-represented in eHealth research? (Glueckauf and Lustria 2008, p.4). The use of telecommunications in relation to accessing health information appeared low because of the low rates of access to telecommunications in the home. However, a total 16 CALD participants reported having access to the Internet and 10 CALD participants reported using the Internet to access health information, this indicates that most of those who had access to the Internet appear to have some experience of using it for this purpose. Likewise, the number of participants who reported not having access to the Internet was similar to the number who reported not using the Internet to access health information, suggesting that use of the Internet to access health information may have been higher if access to the Internet was higher. There were, however, some limitations to the survey.
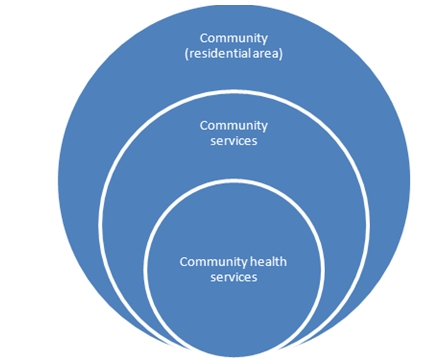
The motivation to access health information via telecommunications may have been linked to the availability of other services seen as a source of information and this should be explored further. This research was conducted in a CHC which was in the centre of the public housing area. The CHC adopts a community health model of care and may be viewed as a hub of health and allied health services. This hub is in very close proximity to the residential areas of the estate; consequently, the distance to community health services was not an issue for most residents. However, this does not necessarily mean that telecommunications holds no value in terms of health information for this community. The National Ethnic Disability Alliance (NEDA) (2010) argued that geographic distance is not in itself a determinant of access to information and communication technology It does, however, suggest that this concept may need to be clearly defined within a community health model, particularly as this is a key part of current health reforms (NHHRC 2009).
Figure 12 ? Diagram showing the proximity of community health services
Culturally and linguistically appropriate health information in a range of languages, regardless of the medium for its delivery
There are a number of constraints in regards to this particular community becoming high users of the Internet to access health information, namely
- Access to Internet in the home is low on the estate
- They have a source of in-person health information at the CHC
- Principle income source is Age or Service pension, followed by Disability Support Pension (Regional Housing Office 2011)
- 34% of people living in public housing properties on the estate are over the age of 55 (Regional Housing Office 2011)
- English language competence
Furthermore, the health professionals who work with this community showed little confidence that the use of telecommunications would be a feasible alternative to face-to-face contact (Fig 11). The reasons for this could be explored in depth in further qualitative research with this group of health professionals.
eHealth initiatives must be grounded in the needs of specific communities and fit the context of health services in the region
Community health services are perceived as an essential part of good practice for meeting the health needs of refugees and migrant populations, particularly for recently arrived refugees (Woodland et al. 2010). The findings of this study are encouraging in the sense that there was evidence that CALD participants were satisfied with their community health services and were recruited for the survey while present at the CHC.
These preliminary findings support the argument that analyses of cultural preferences within eHealth must extend beyond simply focusing on access to telecommunications and take into account other factors such as availability and familiarity with technologies in countries of origin (Leung 2011), and availability of translated information in Australia. Australia?s multicultural population will increasingly require bilingual, culturally-competent health workers who act as the bridge between the Australian health care system and CALD communities, regardless of whether face-to-face contact occurs (Greenstock et al. 2013). This principle applies just as much to the delivery of health information via telecommunications and an important next step is exploring the system requirements of achieving this.
Attention must be paid to the changing relationships between patients and health professionals as new models of care are introduced. Research is needed to explore the extent to which various patient populations view themselves as active agents and are motivated to seek health information, as well as the emerging role of the health professional as broker or facilitator of electronic information. The latter has considerable implications for job roles and training. In addition, the use of telecommunications in health services must be diversified to differentiate for different client groups and models of service delivery. A community health services hub model could make use of telecommunications in a very different way to health services for rural and remote areas but there is potential for enabling quality health care ? and access to clinically accurate information - with telecommunications in both contexts.
Study limitations
There were a number of limitations in this exploratory study. The challenges in defining terms in an exploratory research area meant that use of the term ?health information? was at times inconsistent and a source of some confusion. This was reflected in the questions that were included, and not included, in the survey. This affected the depth and quality of the survey findings. A more concise definition of health information and the role of health professionals in delivering this information was needed. Selecting a community or communities to work with was also challenging. Conducting this study confirmed to the research team that the term CALD encompasses an extremely wide variety of heterogeneous communities and it, therefore, proved most reasonable to adopt a community survey approach which was not able to generate generalisable results. The experience also confirmed that time commitment must be considered when planning this kind of research, taking into account the need to gain the trust of the community and any gatekeepers involved.
Further limitations surrounded the development of the survey instrument. The pilot survey was found to be too long and the final survey was revised and shortened. A consequence of keeping the survey to a reduced length meant that it was not possible to drill down into some aspects of telecommunications access and usage, which in turn, also affected the quality of the data.
The experience of identifying these limitations have, however, provided very useful insights in line with the expectations of an exploratory study with a culturally diverse community.
Conclusion
This study sought to explore the extent to which a CALD community group had access to telecommunications in the home. The intention of the study was to investigate the extent of the use of telecommunications technologies to access health information. The study indicated that access to telecommunications was lower than the State average and that use of these technologies, where available, to access health information was also low. However, the findings also indicated that some of those who did have access to the Internet did use it for accessing health information, while some of those who didn?t use the Internet for this purpose didn?t have access to the Internet in the home. There is a window of opportunity here to determine whether the use of the Internet to access health information would increase if access to the Internet were to also increase. This would depend on a thorough understanding of the reasons for the low levels of Internet access, which we believe would be more complex than affordability alone and are likely to include personal choice and cultural preferences. As the Internet continues to evolve to incorporate developments in multimedia and audio, it would be timely to explore the extent to which this may also enable access to information for non-native English speakers.
Concerns have been raised around the extent to which eHealth policy has been adapted to meet the needs of a multicultural community (NEDA 2010). The need for health-related information may in itself be influenced by the proximity and availability of health services, typically perceived as a source of health information by some communities. Universal access to electronic health information depends on universal access to the means of accessing this information. However, community health services may provide an important role in addressing gaps and maybe more suited as a source of information for some communities.
Australia?s population will continue to grow in size and diversity, with the population expected to almost double between 2007 and 2056 (ABS 2008). The use of telecommunications will also continue to develop and replace many out-dated service delivery channels (ACMA 2011). Researchers must continue to address the interplay of cultural diversity with innovations in health information and health care, in order to ensure that every effort is made to develop health services that are accessible and acceptable to settled and recently arrived residents of Australia.
References
Australian Bureau of Statistics. 2006. Census Quickstats: Victoria. Accessed 12 May 2012. Available from:
Australian Bureau of Statistics. 2008. 3222.0 - Population Projections, Australia, 2006 to 2101. Latest ISSUE Released at 11:30 AM (CANBERRA TIME) 04/09/2008. Accessed 17 October 2012. Available from: http://www.abs.gov.au/ausstats/abs@.nsf/mf/3222.0
Australian Bureau of Statistics. 2011. Migration, cat. no. 3412.0, ABS, Canberra.
Australian Communications and Media Authority. 2011. Communications report 2010-2011 Series: Report 3 ? The emerging mobile telecommunications service market in Australia. Commonwealth of Australia 2011. Accessed 17 October10 2012. Available from: http://www.acma.gov.au/webwr/_assets/main/lib410148/CommsRep3_Emerging_mobile_tcomms_svce.PDF
Colorado State University. 2013. ?Writing Guides?. [Internet] Accessed 23 January 2013. Available from: http://writing.colostate.edu/guides/index.cfm
Community Indicators Victoria. 2011. Indicator: Home Internet Access by LGA. Accessed 24 May 2012. Available from: http://www.communityindicators.net.au/files/civ/instant_atlas_wellbeing/map.html
Department of Health Victoria. 2009. Putting patients first: Working in partnership to deliver a better Australian health system. ISBN 978-1-921697-05-0.
Denizard-Thompson, NM; Feiereisel, KB; Stevens, SF; Miller, DP; Wofford; JL. .2011. ?The Digital Divide at an Urban Community Health Center: Implications for Quality Improvement and Health Care Access?. Journal of Community Health 36 (3): 456-460. http://dx.doi.org/10.1007/s10900-010-9327-5
Glueckauf, R.; Lustria, M. 2008. eHealth Intervention Outcome Research: Will it Benefit Underserved Rural and Ethnic Minority Populations? Conference Papers -- International Communication Association: 1-21.
Greenstock, L; Woodward-Kron, R; Fraser, C; Naccarella, L; Elliott, K; Bingham, A; Morris, M. 2013. The role of telecommunications for communicating health information to migrant communities. ?Journal of Public Health Research?. 1(3): e34
Henderson, S; Kendall, E; See, L. 2011. The effectiveness of culturally appropriate interventions to manage or prevent chronic disease in culturally and linguistically diverse communities: a systematic literature review. ?Health & Social Care in the Community?. 19(3): 225-249. http://dx.doi.org/10.1111/j.1365-2524.2010.00972.x
Katz, MG; Jacobson, TA; Veledar, E; Kripalani, S. 2007. Patient literacy and question-asking behavior during the medical encounter: a mixed-methods analysis. ?Journal of General Internal Medicine?. 22(6): 782-6. http://dx.doi.org/10.1007/s11606-007-0184-6
Leung, L. 2011. Mind the Gap: Refugees and communications technology literacy. Report supported by ACCAN. Accessed 13 June 2012. Available from: http://accan.org.au/files/Reports/Mind%20the%20Gap%20ACCAN-UTS.pdf.
Lupton, D. 1997. ?Consumerism, reflexivity and the medical encounter?. Social Science and Medicine, 45(3):373-381. http://dx.doi.org/10.1016/S0277-9536(96)00353-X
Marmot, M. 2005. ?Social determinants of health inequalities?. The Lancet. 364(9464): 1099-1104
McGuirk, P.; Argent, N. 2011. ?Population growth and change: Implications for Australia?s cities and regions?. Geographical Research. 49(3): 317-335. http://dx.doi.org/10.1111/j.1745-5871.2011.00695.x
National Ethnic Disability Alliance (NEDA). 2010. Communicating Difference: Understanding Communications Consumers from Non English Speaking Backgrounds (NESB). A consumer research report supported by the Australian Communications Consumer Action Network (ACCAN).
National Health and Hospital Reform Commission (NHHRC). 2009. A Healthier Future For All Australians ?Final Report, Commonwealth of Australia. Accessed 22 October 2012. Available from: http://www.health.gov.au/internet/nhhrc/publishing.nsf/Content/nhhrc-report.
NBNCo. 2010. Frequently asked questions. . Accessed 24 May 2012. Available from: http://www.nbn.gov.au/frequently-asked-questions/#faq-id-22
Public Health Information Development Unit. 2008. A social health atlas of Australia (third edition online). 2008. Accessed 20 May 2012. Available from: http://www.publichealth.gov.au/data/
Renzaho, A. 2008. ?Re-visioning cultural competence in community health services in Victoria?. Australian Health Review. 32(2): 223-235. http://dx.doi.org/10.1071/AH080223
Richmond Housing Office. 2011. Unpublished Working Document. Richmond VIC.
Sillence, E; Briggs, P; Harris, P; Fishwick, L. 2007. Going online for health advice: Changes in usage and trust practices over the last five years. ?Interacting with Computers?. 19(3):397-406. http://dx.doi.org/10.1016/j.intcom.2006.10.002
Skinner, D; Rendall, K; Andrews G. 1997. ?Community surveys: the benefits and sacrafices. Curationis. 20(1): 21-5
Rudd, R; Keller, D. Health literacy: new developments and research. Journal of Communication in Healthcare. 2009; 2(3):240-57. http://dx.doi.org/10.1179/175380609790912689
Starfield, B. 1994. ?Is primary care essential?? The Lancet. 344: 1129-1133. http://dx.doi.org/10.1016/S0140-6736(94)90634-3
Sulaiman-Hill, C; Thompson, S. 2011. ?Sampling challenges in a study examining refugee resettlement?. BMC International Health and Human Rights. 11:2. Accessed 23 January 2013. Available from: http://www.biomedcentral.com/content/pdf/1472-698X-11-2.pdf . http://dx.doi.org/10.1186/1472-698X-11-2
Woodland, L; Burgner, B; Paxton, G; Zwi, K. 2010. ?Health service delivery for newly arrived refugee children: A framework for good practice?. Journal of Paediatrics and Child Health. 46. 560-567. http://dx.doi.org/10.1111/j.1440-1754.2010.01796.x
Zainal, Z. 2007. Case study as a research method. Jurnal Kemanusiaan bil. 9. Accessed 6 September 2012.
Available from: http://eprints.utm.my/8221/1/ZZainal2007-Case_study_as_a_Research.pdf
Appendix 1
Connecting people from culturally and linguistically diverse (CALD) backgrounds and health professionals through telecommunications
This survey is about your use of telephone, mobile phone and internet, the ways in which health information and services are made available to you, and how you communicate with health professionals (doctors, nurses, speech pathologists). Your answers are anonymous and will be kept confidential. By returning this pilot survey your consent to take part is implied. Thank you for your participation.
General Information
Male ? Female ? Age: ____________
First language: ____________________ Other languages: _______________
How long have you lived in Australia? ___________________
How often do you visit a health professional (e.g. doctor, nurse, speech pathologist)? ____________________________________
Do you use any of the following at home? (please tick all that apply)
? Landline telephone
? Mobile telephone
? Internet
? Email
How often do you use the internet? ? Everyday ? Sometimes ? Never
How often do you use a landline telephone?? Everyday ? Sometimes ? Never
How often do you use a mobile telephone?? Everyday ? Sometimes? Never
Landline telephone
Please tick the statements that apply to you (please tick all that apply)
? I know how to make and answer calls on a landline phone
? I use a landline telephone to find information about my health
? I use a landline telephone to find health services (doctor, nurse, specialist)
? I use a landline telephone to arrange appointments with health professionals
? I use a landline telephone to ask questions of a health professional
? I have consultations with a health professional on a landline telephone
? Health professionals contact me on my landline telephone
Mobile telephone
? I know how to make and answer calls on a mobile phone
? I know how to send and receive text message on a mobile phone
? I know how to send and receive emails on a mobile phone
? I use a mobile telephone to find information about my health
? I use a mobile telephone to find health services (doctor, nurse, specialist)
? I use a mobile telephone to arrange appointments with health professionals
? I use a mobile telephone to ask questions of a health professional
? I have consultations with a health professional on a mobile telephone
? Health professionals contact me on my mobile telephone
Computer and the Internet
? I know how to send and receive emails
? I know how to search the internet and find websites
? I know how to talk to people using Skype or other online video services
? I use the internet to find information about my health
? I use the internet to find health services (doctor, nurse, specialist)
? I use the internet to arrange appointments with health professionals
? I use the internet to ask questions of a health professional
? I have consultations with a health professional using the internet
? Health professionals contact me via the internet
? Health professionals contact me another way (e.g. by post)
? Health professionals don?t contact me at all
Please tick the statements that apply to you (please tick all that apply)
? I have found health information in a language I can read
? I have found health information on the internet in a language I can read
? I have been able to talk to a health professional in a language I understand
? I have been able to use the telephone to find health information in a language I understand
How often do you use an interpreter service when communicating with a health professional? (tick one)
? Always ? Sometimes ? Never
How often do you use a telephone interpreter service when communicating with a health professional? (tick one)
? Always ? Sometimes ? Never
Are you satisfied with your communication with health professionals and health services?
? Satisfied ? Somewhat satisfied ? Dissatisfied
This project was funded by ACCAN
Appendix 2
Connecting people from culturally and linguistically diverse (CALD) backgrounds and health professionals through telecommunications
Survey for health professionals
This survey is about your general use of telecommunications (telephone and internet) in the workplace, the ways in which health information and services are made available by you, or the service you work for, to people from CALD communities, and how you communicate with patients from CALD communities. Your answers are anonymous and will be kept confidential. By returning this pilot survey your consent to take part is implied. Thank you for your participation.
General Information
Gender: ____________________ Age: _________
First language: ______________________ Second language: ________________
Job title: __________________________________
Were you born in Australia?__________________________
If no, for how long have you lived in Australia?
I have access to the following telecommunications in the workplace (please have in mind the workplace where you base yourself most often) (please tick all that apply)
? Landline telephone
? Mobile telephone
? Internet
? Email
How often do you use the internet? ? Everyday ? Sometimes? Never
How often do you use a landline telephone? ? Everyday ? Sometimes ? Never
How often do you use a mobile telephone? ? Everyday ? Sometimes? Never
I feel that learning more about how to use the following telecommunications would help me in my professional role (please tick all that apply)
? Landline telephone
? Mobile telephone
? Internet
? Email
Landline telephone
(Please tick the all the statements that apply to you in your professional role)
? I know how to make and answer calls on a landline phone
? I use a landline telephone to arrange appointments with patient
? I use a landline telephone to ask patients questions
? I use a landline telephone for consultations with patients
? Patients contact me on my landline telephone at work
? Patients contact me on my landline telephone at home
Mobile telephone
? I know how to make and answer calls on a mobile phone
? I know how to send and receive text message on a mobile phone
? I know how to send and receive emails on a mobile phone
? I use a mobile telephone to arrange appointments with patients
? I use a mobile telephone to ask patients questions
? I use a mobile telephone for consultations with patients
? Patients contact me on my mobile telephone
Computer and the Internet
? I know how to send and receive emails on a computer
? I know how to search the internet and find websites
? I know how to talk to people using Skype or other online video services
? I use the internet to arrange appointments with patients
? I use the internet to ask patients questions
? I use the internet for consultations with patients
? Patients contact me via the internet
? Other _________________________
? Patients contact me another way (e.g. by post)
?Patients don?t contact me directly
How often do you use an interpreter service when communicating with patients? (tick one)
? Always ? Sometimes ? Never
How often do you use a telephone interpreter service when communicating with patients? (tick one)
? Always ? Sometimes ? Never
What strategies do you use to facilitate communication with patients from culturally and linguistically diverse backgrounds?
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
What strategies do you use to share or signpost health information with patients from culturally and linguistically diverse backgrounds?
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
Do you feel telecommunications (telephone and/or internet) could enable better communication with patients from culturally and linguistically diverse backgrounds?
? Yes ? No ? Maybe
Please explain your answer
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
___________________________________________________________________________
Additional comments
Please share any additional comments.
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
________________________________________________________________________
Thank you for taking the time to fill out our survey. Your input is greatly appreciated. Please feel free to contact us if you have any further questions.